Semaglutide Slows Epigenetic Aging in People with HIV-associated Lipohypertrophy
Trial Title
Semaglutide Slows Epigenetic Aging in People with HIV-associated Lipohypertrophy: Evidence from a Randomized Controlled Trial
Collaborating Institutions University
University Hospitals Cleveland Medical Center; Case Western Reserve University; Yale University School of Medicine
Summary Snapshot
Study Type: Double-blind, placebo-controlled randomized controlled trial (post-hoc epigenetic analysis)
Sample Size: 108 participants (84 with paired epigenetic data: 45 semaglutide, 39 placebo)
Duration: 32 weeks
Primary Endpoint: Change in epigenetic age acceleration (EAA) across DNA methylation clocks
The DNA Methylation Edge
DNA methylation enabled sensitive, system-level detection of aging changes that traditional clinical endpoints would miss. By applying multiple generations of epigenetic clocks and organ-specific aging measures to paired samples, this study captured semaglutide’s broader geroprotective signal in a high-risk population.
Objective & Rationale
Study goal and scientific context: The study aimed to assess semaglutide's effects on epigenetic aging biomarkers in adults with HIV-associated lipohypertrophy via post-hoc analysis of a phase 2b RCT, using multiple DNA methylation clocks to measure biological aging changes over 32 weeks. It addressed accelerated aging in people with HIV (PWH) due to chronic inflammation and metabolic issues, where semaglutide (a GLP-1 agonist) might mitigate these symptoms via weight loss and anti-inflammatory effects. Findings help establish how epigenetic clocks predict morbidity/mortality and how slowing aging could extend the healthspan in high-risk populations with limited gerotherapeutic options.
Methodology
- Design: Double-blind, placebo-controlled phase 2b RCT; post-hoc analysis of paired PBMC methylomes; ANCOVA for group differences adjusted for confounders; EWAS via limma
- Population: Adults ≥18 with HIV-1 on stable ART (HIV RNA <400 copies/mL), BMI ≥25, lipohypertrophy (waist >95/94 cm men/women, waist-to-hip >0.94/0.88); mean age 49±12, 58% Black, 42% women; exclusions: diabetes, CVD, pregnancy
- Intervention: Once-weekly subcutaneous semaglutide (titrated: 0.25 mg weeks 1-4, 0.5 mg weeks 5-8, 1.0 mg thereafter) vs. placebo
- Duration: 32 weeks (with sampling at baseline and week 32)
- Epigenetic Measurements: Infinium MethylationEPIC BeadChip; preprocessing with minfi/ENmix (GMQN normalization, BMIQ, knn imputation); clocks: first-gen (PC Horvath pan tissue/skin-blood, PC Hannum); second-gen (PC PhenoAge, GrimAge V1/V2); third-gen (DunedinPACE); others (OMICmAge, RetroAge, DNAmTL, SystemsAge with 11 organ clocks, Intrinsic Capacity); annualized EAA changes
Key Findings
- Results: Semaglutide significantly reduced epigenetic aging vs. placebo across multiple clocks (e.g., PCGrimAge, DunedinPACE, PhenoAge), with concordant slowdowns in 11 organ-system clocks (e.g., inflammation, brain, heart) but no observed change in Intrinsic Capacity. Telomere length shortened slightly; findings suggest semaglutide possesses geroprotective effects beyond weight loss, potentially via reduced inflammation.
- Standard Metrics: % change in biological age, direction of effect, significance PCGrimAge EAA: -3.08 years/year; DunedinPACE: -0.09 units/year; GrimAge V1: -1.39 years/year; GrimAge V2: -2.26 years/year; PhenoAge: -4.90 years/year; OMICmAge: -2.20 years/year; RetroAge: -2.18 years/year; SystemsAge: -4.17 years/year; DNAmTL: -0.04 years/year.
- Academic Significance: Though pharmacologic agents developed for improved metabolic outcomes, including GLP-1, are known to affect both metabolic regulation and aging, little research to date has established whether or not GLP-1 receptor agonists such as semaglutide can reduce inflammation and affect biological aging processes (while also reducing weight).
- Clinical Significance: This study is among the first to demonstrate potential gerontotherapeutic and geroprotective outcomes from prescribing semaglutide to populations at high risk of inflammation and accelerated biological aging. Clinical outcomes may be attributed to GLP-1 receptor agonists’ ability to reduce visceral fat, thereby reducing inflammation-related aging and impacting aging cascades.
Extending Trial Insights from Aging to Companion Diagnostics
One of the most powerful attributes of DNA methylation (DNAm) data is its depth: a single dataset can support multiple layers of insight when paired with well-designed algorithms. Beyond measuring how GLP-1 therapies influence biological aging, DNAm can be used to anticipate who benefits, how, and at what potential cost.
The Clinical Question Behind GLP-1s
GLP-1 receptor agonists are highly effective for weight loss and glycemic control, but emerging evidence suggests that a meaningful portion of weight loss, particularly in older adults, may come from lean muscle mass, not just adipose tissue. In aging populations already vulnerable to sarcopenia and frailty, this raises an important question: Are we improving metabolic health at the expense of functional capacity?
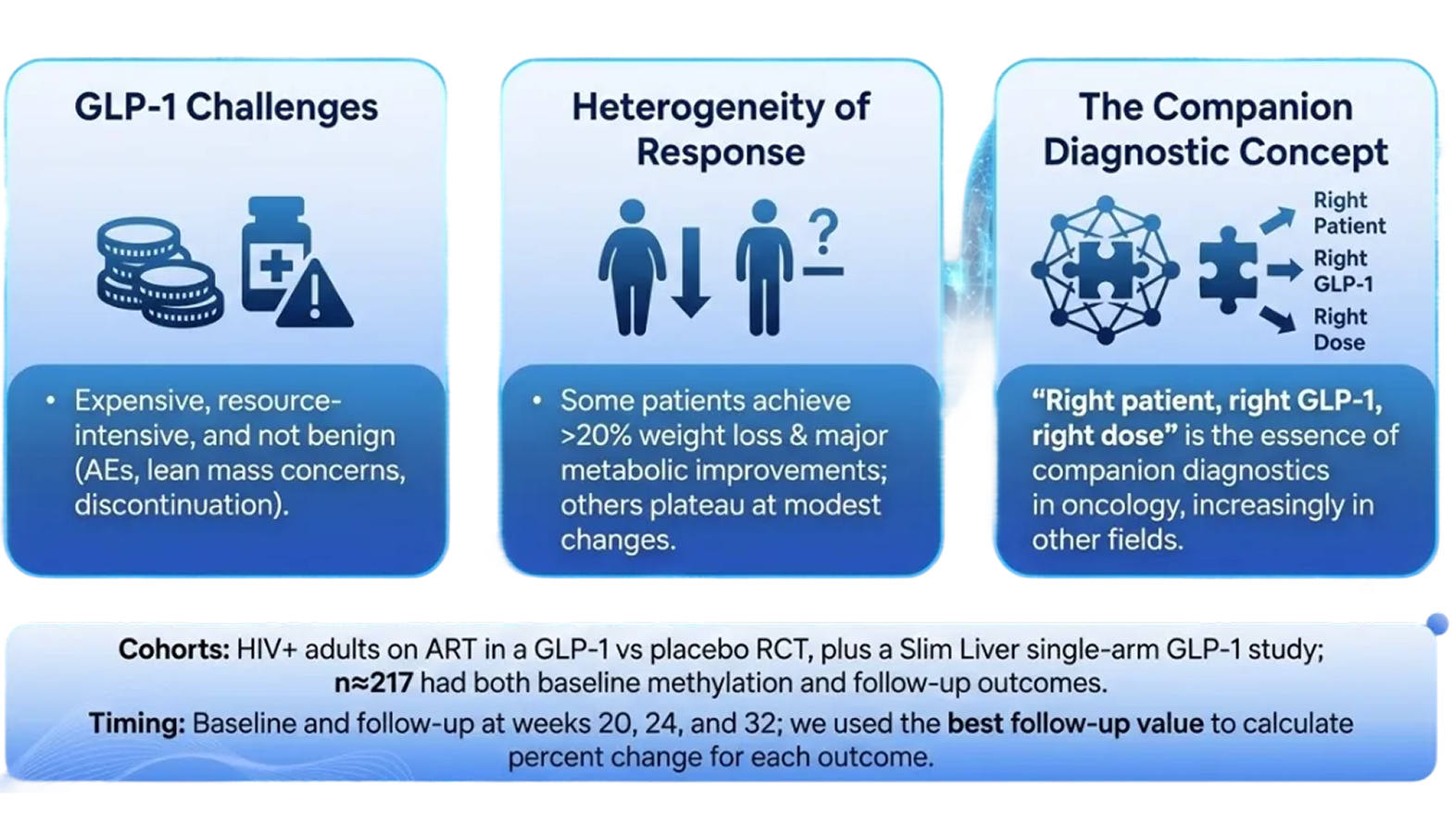
Using DNAm as a Predictive Companion Diagnostic
We hypothesized that DNAm could address this tradeoff proactively – not as a retrospective biomarker, but as a predictive companion diagnostic to guide therapy selection and monitoring. Similar approaches are now standard in oncology and precision medicine; we believe metabolic therapeutics are next.Using DNAm data from this randomized controlled trial, we developed algorithms to predict multiple GLP-1–associated response domains, including:
- Primary metabolic response (BMI, HbA1c, insulin resistance)
- Visceral and trunk fat reduction (DXA-derived)
- Inflammatory response (hsCRP, sCD163, sCD14)
- “Super-responder” profiles combining metabolic and inflammatory improvement
- BMI-dominant weight loss phenotypes
As expected, DNAm models successfully predicted weight loss and glycemic improvement. Importantly, the signal extended beyond traditional metabolic endpoints: DNAm also predicted reductions in coronary artery calcium, a robust marker of cardiovascular risk and mortality.
.png)
Why This Matters
These findings expand DNAm’s role from descriptive measurement to decision support. Rather than optimizing for weight loss alone, DNAm-based companion diagnostics could help identify individuals most likely to achieve durable metabolic and cardiovascular benefit while flagging those who may require adjusted dosing, resistance training, nutritional support, or alternative interventions to preserve lean mass and function.
.png)

.png)
.png)
.png)
.png)